Blog 
Click here to go back
HOT TOPICS: Provider Guidance for Medicaid Renewals
Provider Role in Medicaid Renewals
DMS encourages providers to support their patients undergoing renewals in the following ways:
When is their renewal?
Ensure patients know when their renewal due date is and to be on the lookout for notices from KY Medicaid. Encourage them to keep their contact information current in kynect, including mailing address, telephone number and email address.
How to renew?
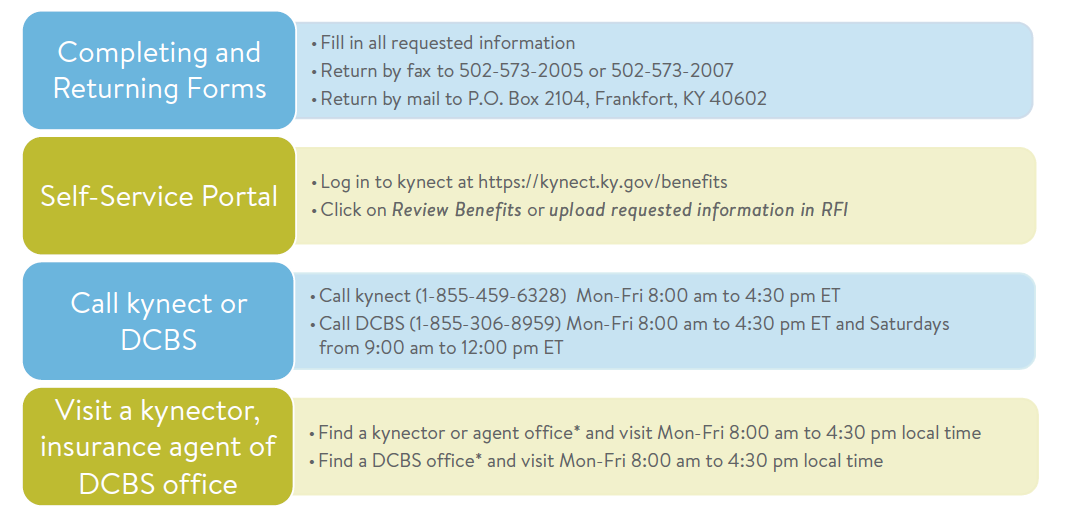
Guide patients in completing the steps necessary to respond to notices requiring action before their renewal due date. Help them understand what steps to take to upload information. Connect patients to state-employed kynectors, insurance agents, or state-certified navigators for assistance if needed. Providers may utilize content on the KY Public Health Emergency Unwinding website to support understanding of actions to be taken.
What to do if they are administratively terminated?
While the state is taking steps to ensure that this won’t happen, there may be some patients whose coverage ends even though they may be eligible for Medicaid. A lack of providing information or response prior to their renewal due date will lead to DMS being unable to determine eligibility and renew their coverage. For these patients, providers are encouraged to connect these individuals with kynectors, insurance agents, or state-certified navigators to support them in identifying and submitting all necessary materials for redetermination. If done within 90 days after their end date, the patient could be retroactively reinstated without a gap in coverage. Patients also have 90 days to appeal the administrative termination.
What if they are determined ineligible?
For patients discontinued due to no longer being Medicaid eligible, providers may help individuals understand alternative options for health care coverage, including the state’s Qualified Health Plans (QHPs) available at kynect.ky.gov. Connect patients to state-employed kynectors, insurance agents and state-certified navigators to assist.
PHE Renewal Plan
The state anticipates completing renewals for over 1.6 million individuals. The KY Medicaid renewal process will start in April for those individuals with a renewal due by May 31, 2023. DMS will send notices to individuals going through renewals no fewer than 60-days in advance of their renewal date. Through working closely with patients, providers can determine the specific circumstances for their ongoing renewal and support them in understanding the importance of completing the steps required and ways to do so.
Renewals will follow one of three paths:
Passive Renewals.
Medicaid members for which DMS can verify eligibility through existing data sources will be “passively” renewed. Rather than receive a renewal package, individuals who are passively renewed will receive a Notice of Eligibility. Individuals will not be required to take any further action.
Request for Information.
If the state is unable to verify information, an individual may receive a Request for Information (RFI) to support the renewal process. The individual will need to take action by verifying information before eligibility is re-determined.
Active Renewals.
Medicaid members for which DMS does not have sufficient information available to determine the individual’s eligibility will receive a Renewal Packet 60 days in advance of their eligibility review. Individuals will need to take action to upload additional documentation to support re-determining their eligibility.
PHE Renewal Caseload Mix
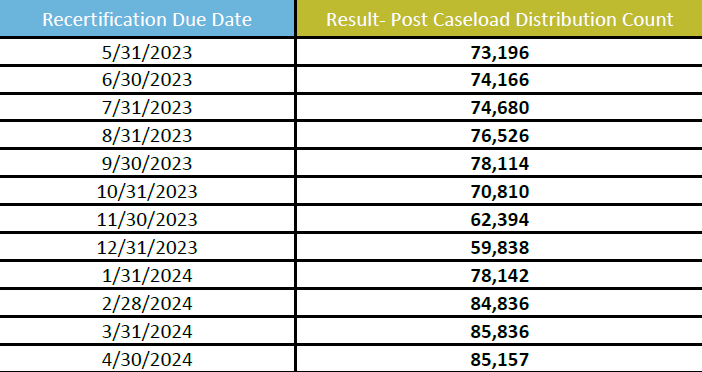
The caseload of individuals requiring active renewal will be distributed across a 12-month period (May 2023 – April 2024). DMS’ Renewal Distribution Plan has aligned renewal dates for members of the same household as well as aligned Medicaid and SNAP renewal dates.
DMS has prioritized the following populations:
• Medicare-eligible (May to October)
• QHP-eligible (July to April)
• Children under 19 years of age (July to April)
All other populations will be assigned a month for renewal based on the state’s random renewal realignment algorithm. The table below provides the anticipated caseload breakdown, as a percentage of the total population, for the 12-month renewal timeline.
How to Help Patients During the Renewal Process
While working with patients, providers are encouraged to connect their patients to supports in the community to make sure they know how to respond to any notices. There are numerous ways to submit information and many people in the community that can help.